Vol 5 No 2 (2010)
Articles
-
Clinicians should be aware of new developments to familiarize themselves with pharmacokinetic and pharmacodynamic characteristics of new anticoagulant agents to appropriately and safely use them. For the moment, cardiologists and other clinicians also require to master currently available drugs, realizing the mechanism of action, side effects, and laboratory monitoring to measure their anticoagulant effects. Warfarin and heparin have narrow therapeutic window with high inter- and intra-patient variability, thereby the use of either drug needs careful laboratory monitoring and dose adjustment to ensure proper antithrombotic protection while minimizing the bleeding risk. The prothrombin time (PT) and the activated partial thromboplastin time (aPTT) are laboratory tests commonly used to monitor warfarin and heparin, respectively. These two tests depend highly on the combination of reagent and instrument utilized. Results for a single specimen tested in different laboratories are variable; this is mostly attributable to the specific reagents and to a much lesser degree to the instrument used. The PT stands alone as the single coagulation test that has undergone the most extensive attempt at assay standardization. The international normalized ratio (INR) was introduced to ‘‘normalize’’ all PT reagents to a World Health Organization (WHO) reference thromboplastin preparation standard, such that a PT measured anywhere in the world would result in an INR value similar to that which would have been achieved had the WHO reference thromboplastin been utilized. However, INRs are reproducible between laboratories for only those patients who are stably anticoagulated with vitamin K antagonists (VKAs) (i.e., at least 6 weeks of VKA therapy), and are not reliable or reproducible between laboratories for patients for whom VKA therapy has recently been started or any other clinical conditions associated with a prolonged PT such as liver disease, disseminated intravascular coagulation, and congenital factor deficiencies. In contrast to marked progress in the standardization of PT reagents for INR reporting, no standardization system has been globally adopted for standardization of PTT reagents. Recently College of American Pathologists recommend that individual laboratories establish their own therapeutic range by using aPTT values calibrated against accepted therapeutic unfractionated heparin (UFH) levels calibrated against accepted therapeutic UFH levels performing anti-Xa test (which is the most accurate assay for monitoring UFH therapy).
Herein, we review recent data on the monitoring of conventional anticoagulant agents. Marked interlaboratory variability still exists for PT, INR, and PTT tests. Further research should be focused on improving the standardization and calibration of these assays. -
Background: The evaluation of prosthetic valves is very difficult with two-dimensional transthoracic echocardiography alone. Doppler and color flow imaging as well as transesophageal echocardiography are more reliable to detect prosthetic valve dysfunction. However, Doppler study sometimes tends to be misleading due to the load-depending characteristics of peak and mean pressure gradients. The peak-to-mean pressure decrease ratio is a load-independent measure, which was previously used for the detecting and grading of aortic valve stenosis. We assessed the usefulness of this method for the evaluation of aortic valve prosthesis obstruction.
Methods: One hundred fifty-four patients with aortic valve prostheses were included in this study. Transthoracic and transesophageal echocardiographic examinations were performed in all the patients. Peak velocity and velocity time integral of the aortic valve and left ventricular outflow tract, peak and mean aortic valve pressure gradients, peak-to-mean pressure gradient ratio, and time velocity integral (TVI) index were measured.
Results: There was a significant relation between the TVI index (p value < 0.001) and aortic prosthesis obstruction. A TVI index < 0.2 had a sensitivity of 71% and specificity of 100% for the detection of aortic valve prosthesis obstruction. However, no significant relation was found between the peak-to-mean pressure ratio and aortic valve prosthesis obstruction (p value = 0.09).
Conclusion: Although the peak-to-mean pressure gradient (PG/MG) ratio is a simple, quick, and load-independent method which may be useful for the grading of aortic valve stenosis, it is poorly associated with aortic valve prosthesis obstruction. The TVI index is a useful measure for the detection of aortic prosthesis obstruction. -
Background: Transcatheter closure of atrial septal defect secundum (ASD-II) has become an alternative method for surgery. We sought to compare the two-dimensional transesophageal echocardiography (TEE) method for measuring atrial septal defect with balloon occlusive diameter (BOD) in transcatheter ASD-II closure.
Methods: A total of 39 patients (71.1% female, mean age: 35.31 ± 15.37 years) who underwent successful transcatheter closure of ASD-II between November 2005 and July 2008 were enrolled in this study. Transthoracic echocardiography (TTE) and TEE were performed to select suitable cases for device closure and measure the defect size before the procedure, and BOD measurement was performed during catheterization via TEE. The final size of the selected device was usually either equal to or 1 – 2 mm larger than the BOD of the defect.
Results: The mean defect size obtained by TEE and BOD was 18.50 ± 5.08 mm and 22.86 ± 4.76 mm, respectively. The mean difference between the values of ASD size obtained by TEE and BOD was 4.36 ± 2.93 mm. In comparison with BOD, TEE underestimated the defect size in 94.9%, but TEE value being equal to BOD was observed in 5.1%. There was a good linear correlation between the two measurements: BOD = 0.773 × ASD size by TEE+8.562; r2 = 67.9.1%. A negative correlation was found between TEE sizing and the difference between BOD and TEE values (r = -0.394, p value = 0.013).
Conclusion: In this study, BOD was larger than ASD size obtained by two-dimensional TEE. However, TEE maximal defect sizing correlates with BOD and may provide credible information in device size selection for transcatheter ASD closure. -
Background: Recent interests have mainly focused on the roles of serum calcium and phosphorus and their product (Ca-P product) in the development of valvular heart disease. The present study assessed the relationship between the Ca-P product and the severity of valvular heart disease in end-stage renal disease (ESRD) patients undergoing chronic hemodialysis.
Methods: This cross-sectional study reviewed the clinical course of 72 consecutive patients with the final diagnosis of ESRD candidated for chronic hemodialysis. The severity of valvular heart disease was determined using M-mode two-dimensional echocardiography. The serum calcium and phosphate values adopted were those values measured on the day between the two consecutive dialyses, and the Ca-P product was calculated.
Results: The most common causes of ESRD were diabetic nephropathy, malignant hypertension, and chronic glomerulonephritis. The mean Ca-P product level in the dialysis patients was 50.44 ± 17.78 mg2/dL2. The receiver-operator characteristic (ROC) curve illustrated that a Ca-P product level > 42 mg2/dL2 was the optimal value in terms of sensitivity and specificity for predicting the presence of valvular insufficiency. Aortic insufficiency was directly associated with a high Ca-P product value after adjustment for age, gender, serum albumin, diabetes, hypertension, hyperlipidemia, coronary artery disease, and serum creatinine (β = 0.412, SE = 158, p value= 0.011).
Conclusion: A positive relationship between the Ca-P product value and the severity of aortic insufficiency is expected. Achieving an appropriate control of the Ca-P product level may decrease aortic valve calcification and improve the survival of patients on chronic hemodialysis. -
Sonographic Prediction of Body Fat Volume (Subcutaneous and Visceral Fat) in Cardiovascular Patients
Introduction: Inappropriate body composition represents impaired energy and nutrient intake and can be a risk factor for many diseases, especially for cardiovascular disease. Different methods have been suggested for the estimation of body fat volume and its distribution. However, they may be either expensive or hazardous for some groups of patients. Sonography is a very accessible technique, which may be used for the evaluation of visceral and subcutaneous fat volume. The purpose of this study was to evaluate the sonographic prediction of body fat and its distribution in subcutaneous and visceral compartments.
Methods: During a three-month period, we conducted sonographic evaluations for visceral and subcutaneous fat in 106 patients who were admitted to our hospital. The subcutaneous fat was measured at the para-umbilical region and visceral fat was measured in the right para-renal space. The results were compared with the data obtained from the body mass index (BMI) and bioelectric impedance analysis.
Results: The mean age of the patients was 58.8 years, and the mean BMI was26.48 ± 0.33. The mean values of fat percent and fat mass obtained by the electric-method were 31.07 ± 0.81% and 22.12 ± 0.68 kg, respectively. The respective mean values of subcutaneous and visceral fat obtained by sonography were 20.50±0.56 mm and 24.14 ± 0.58 mm. The correlation between BMI and subcutaneous fat was 0.85 (p value < 0.0001) and the correlation between BMI and visceral fat was0.46 (p value < 0.0001).
Conclusion: Sonography is a reliable and available method for the estimation of body fat and its distribution in cardiovascular patients, in subcutaneous and visceral compartments. -
Background: Radiofrequency catheter ablation (RFCA) has been introduced as the treatment of choice for supraventricular tachycardia. The aim of this study was to evaluate the success rate as well as procedural and in-hospital complications of RFCA for the treatment of atrioventricular nodal reentrant tachycardia (AVNRT).
Methods: Between March 1995 and February 2009, 544 patients (75.9% female, age: 48.89 ± 13.19 years) underwent 548 RFCAs for AVNRT in two large university hospitals. Echocardiography was performed for all the patients before and after the procedure. Electrocardiograms were recorded on digital multichannel systems (EP-Med) or Bard EP system. Anticoagulation was initiated during the procedure.
Results: From the 548 patients, 36 had associated arrhythmias, atrial flutter (4%), atrial fibrillation (0.7%), concurrent atrial fibrillation and atrial flutter (0.7%), and concealed atrioventricular pathway (0.4%). The overall success rate was 99.6%. There were 21 (3.9%) transient III-degree AV blocks (up to a few seconds) and 4 (0.7%) prolonged II- or III-degree AV blocks, 2 (0.25%) of which required permanent pacemaker insertion, 3(0.5%) deep vein thrombosis, and one (0.2%) arteriovenous fistula following the procedure. No difference was observed in the echocardiography parameters before and after the ablation.
Conclusion: RFCA had a high success rate. The complication rate was generally low and in the above-mentioned centers it was similar to those in other large centers worldwide. Echocardiography showed no difference before and after the ablation. The results from this study showed that the risk of permanent II or III-degree AV block in patients undergoing RFCA was low and deep vein thrombosis was the second important complication. There was no risk of life-threatening complications. -
Splenomegaly-induced thrombocytopenia is fully described in hematological and surgical literature, but its association with severe aortic stenosis is rare. We present a case of severe aortic valve stenosis with severe splenomegaly-induced thrombocytopenia in which aortic valve replacement was done with a number 23 homograft and splenectomy was performed after the end of cardiopulmonary bypass. Platelet count turned to normal value post-operatively, and the patient spent an ordinary convalescence period and was discharged from the hospital without any complications.
-
Quadricuspid aortic valve (QAV) is an uncommon congenital anomaly which was an incidental finding during surgery or autopsy in the past. We present the case of a 44-year-old woman with moderately severe aortic regurgitation due to unequal cusp size QAV diagnosed via transesophageal echocardiography. Due to echocardiographic imaging improvement, the diagnosis of QAV is now easier and earlier than the past.
-
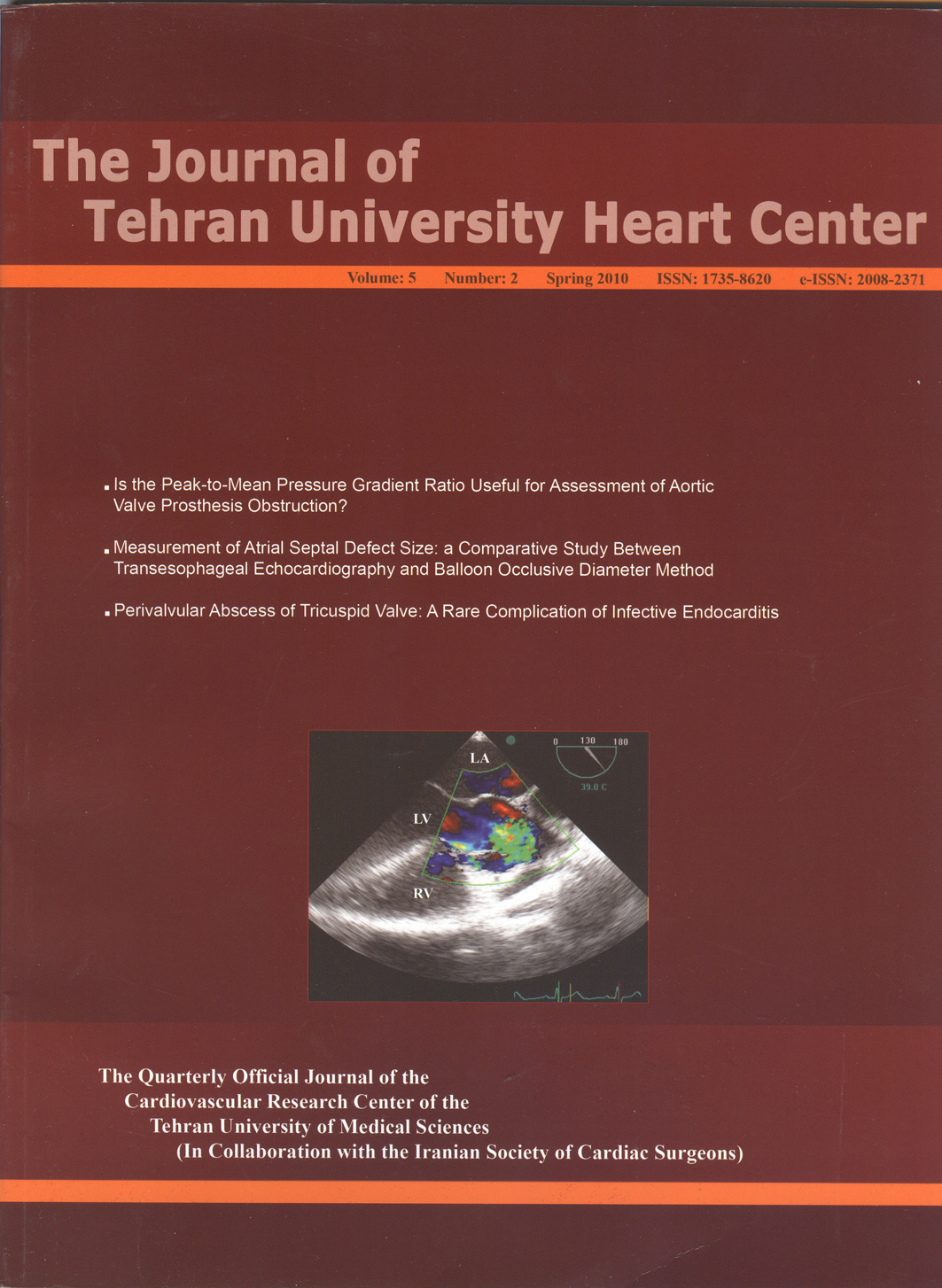
Infective endocarditis is a serious complication of intravenous (IV) drug abuse, with a reported mortality of 5 to 10%. A 21-year-old man, who was an intravenous drug abuser, presented with fever and dyspnea. Transthoracic echocardiography showed a highly mobile, large vegetation on the anterior leaflet of the tricuspid valve. Despite antibiotic therapy for ten days, the patient remained febrile. Transesophageal echocardiography revealed severe aortic regurgitation and an echo-lucent space between the tricuspid and aortic valves. Color Doppler demonstrated a flow within the echo-lucent space and a connection between that and the left ventricle, suggesting a perivalvular abscess of the tricuspid valve opening in the left ventricle. The patient was transferred to the operating room, where he unfortunately expired.