Vol 9 No 4 (2014)
Original Article(s)
-
Background: Several competing geometric and hemodynamic factors are suggested as contributing mechanisms for functional mitral regurgitation (MR) in heart failure patients. We aimed to study the relationships between the severity of MR and the QRS duration and dyssynchrony markers in patients with ischemic or dilated cardiomyopathy.
Methods: We prospectively evaluated 251 heart failure patients with indications for echocardiographic evaluation of possible cardiac resynchronization therapy. All the patients were subjected to transthoracic echocardiography and tissue Doppler imaging to evaluate the left ventricular (LV) synchronicity. The patients were divided into two groups according to the severity of MR: ≤ mild MR and ≥ moderate MR. The effects of different dyssynchrony indices were adjusted for global and regional left ventricular remodeling parameters.
Results: From the 251 patients (74.5% male, mean age = 53.38 ± 16.68 years), 130 had ≤ mild MR and 121 had ≥ moderate MR. There were no differences between the groups regarding the mean age, frequency of sex, and etiology of cardiomyopathy. The LV systolic and diastolic dimensions were greater in the patients with ≥ moderate MR (all p values < 0.001). Among the different echocardiographic factors, the QRS duration (150.75 ± 34.66 vs. 126.77 ± 29.044 ms; p value =0.050) and interventricular mechanical delay (41.60 ± 29.50 vs. 35.00 ms ± 22.01; p value = 0.045) were significantly longer in the patients with ≤ mild MR in the univariate analysis. After adjusting the effect of these parameters on the severity of MR for the regional and global LV remodeling parameters, no significant impact of the QRS duration and dyssynchrony indices was observed.
Conclusion: Our results showed that the degree of functional MR was not associated with the QRS duration and inter- and intraventricular dyssynchrony in our patients with cardiomyopathy. No association was found between the severity of MR and the ischemic or dilated etiology for cardiomyopathy -
Background: About half of all patients who undergo mitral valve surgery suffer from atrial fibrillation (AF). Cox described the surgical cut-and-sew Maze procedure, which is an effective surgical method but has some complications. This study was designed to evaluate the efficacy of a substitution method of radiofrequency ablation (RFA) for patients undergoing mitral valve surgery with AF.
Methods: We evaluated 50 patients, comprising 40 men and 10 women at a mean age of 61.8 ± 7.5 years, who underwent mitral valve surgery with RFA between March 2010 and August 2013. All the patients had permanent AF with an enlarged left atrium (LA). The first indication for surgery was underlying organic lesions. Mitral valve replacement or repair was performed in the patients as a single procedure or in combination with aortic valve replacement or coronary artery bypass grafting. Radiofrequency energy was used to create continuous endocardial lesions mimicking most incisions and sutures. We evaluated the pre- and postoperative LA size, duration of aortic cross-clamping, cardiopulmonary bypass time, intensive care unit stay, and total hospital stay.
Results: The mean preoperative and postoperative LA sizes were 7.5 ± 1.4 cm and 4.3 ± 0.7 cm (p value = 0.0001), respectively. The mean cardiopulmonary bypass time and the aortic cross-clamping time were 134.3 ± 33.7 minand 109.0 ± 28.4 min, respectively. The average stay at the intensive care unit was 2.1 ± 1.2 days, and the total hospital stay was 8.3 ± 2.4 days. Rebleeding was the only complication, found in one patient. There was no early or late mortality. Eighty-two percent of the patients were discharged in normal sinus rhythm. Five other patients had normal sinus rhythm at 6months' follow-up, and the remaining 4 patients did not have a normal sinus rhythm after 6 months.
Conclusion: Radiofrequency ablation, combined with LA reduction, is an effective option for the treatment of permanent AF concomitant with mitral valve surgery. -
Background: Ischemic mitral regurgitation (IMR) is a common complication after acute myocardial infarction (AMI). We aimed to investigate the frequency of IMR following first-time AMI and its association with infarct location, in-hospital mortality, and complications.
Methods: From September 2011 to November 2012, all patients with a diagnosis of first-time acute ST-elevation MI were enrolled in the study. Patients with previous MI and heart failure, organic mitral valve disorders, and previous mitral surgery were excluded from the study. The patients' baseline characteristic, echocardiographic parameters, and complications were recorded. The frequency of IMR after AMI and its relation to infarct location and in-hospital mortality were evaluated.
Results: Altogether, 250 patients (180 male) at a mean age of 60.21 ± 12.90 years were studied. IMR was detected in 114 (45%) patients. There was no association between the presence of MR and gender, systemic hypertension, smoking, diabetes mellitus, or body mass index; however, serum LDL-cholesterol and triglyceride levels were significantly higher in the patients with IMR. The most frequent territory of MI was anterior in the patients without MR, while the anterolateral territory was the most common one in the patients with IMR. The patients with IMR had more reduced left ventricular ejection fraction, more elevated left ventricular end-diastolic pressure, and higher pulmonary arterial pressure (p values < 0.001, < 0.001, and < 0.001, respectively). Stage III diastolic dysfunction was more frequent in the patients with IMR. All the deaths occurred in the IMR patients, who also had more complicated AMI.
Conclusion: IMR following AMI is highly prevalent, and it complicates about half of the patients. Regarding its relation to the AMI complications, assessment of the MR severity is necessary to make an appropriate decision for treatment. -
Background: QT interval parameters have been suggested as a predictor of lethal arrhythmia and mortality in patients with myocardial infarction. The aim of the present study was to compare the value of QT interval indices in patients presenting with non-ST-segment elevation myocardial infarction (NSTEMI) between a group of patients with type 2 diabetes mellitus and a nondiabetic group of patients.
Methods: This case-control study evaluated QT interval parameters in 115 patients (47 diabetic and 68 nondiabetic patients) diagnosed with NSTEMI between September 2011 and July 2012. The following QT interval indices were analyzed: maximum (max) and minimum (min) QT interval; max and min corrected QT interval (QTc); QT dispersion (QTd); and corrected QT dispersion (QTcd). All the patients were observed for ventricular arrhythmia during their hospital course and underwent coronary angiography. They were selected to undergo coronary artery bypass surgery (CABG) or percutaneous coronary angioplasty (PCI) based on their coronary anatomy.
Results: The mean age of the patients was 60.8 ± 11.4 years. The patients were 40.0% female and 60.0% male. There were no significant differences in clinical characters between type 2 diabetic and nondiabetic patients with NSTEMI. Compared with post-myocardial infarction patients without diabetes, those with type 2 diabetes had higher QTc max , QTd and QTcd (p value < 0.05). There was a significant difference in QTd and QTcd in the patients needing coronary revascularization with diabetes as opposed to the nondiabetics (p value = 0.035 and p value = 0.025, respectively) as well as those who had ventricular arrhythmia with diabetes (p value = 0.018 and p value = 0.003, respectively). QTcd was higher in the patients who had higher in-hospital mortality (p value = 0.047). The QTc max, QTd and QTcd were significantly (all p values < 0.05) associated with ventricular arrhythmia, QTcd with need for revascularization and QTc max with in-hospital mortality in the diabetic patients.
Conclusion: Based on the findings of this study, it seems that type 2 diabetics with NSTEMI have greater QTc max, QTd, and QTcd and these QT parameters may have a relationship with worse cardiac outcomes and poorer prognoses. -
Background: Given the lack of consistency in the literature regarding the reliability of the ankle-brachial index (ABI) as a valid screening tool and an independent risk indicator of cardiovascular events and mortality, we compared it with angiography as a reference standard test.
Methods: This case-control study, conducted between 2010 and 2011 in Tehran Heart Center, recruited 362 angiographically confirmed cases of coronary artery disease (CAD) and 337 controls. A standard protocol was used to measure the ABI and different CAD risk factors.
Results: A low ABI had specificity of 99.7%, positive predictive value of 95.8%, negative predictive value of 49.8%, sensitivity of 64%, likelihood ratio of 24.07, and odds ratio (OR) of 22.79 (95%CI: 3.06-69.76). The role of the associated risk factors was evaluated with OR (95%CI), with the variables including gender 3.15 (2.30-4.30), cigarette smoking 2.72 (1.86-3.99), family history 1.72 (1.17-2.51), diabetes 1.66 (1.15-2.4), and dyslipidemia 1.38 (1.02-1.88). In a multivariate model, the following variables remained statistically significantly correlated with CAD [OR (95%CI)]: ABI 13.86 (1.78-17.62); gender 3.69 (2.43- 5.58); family history of CAD 2.18 (1.41-3.37); smoking 1.69 (1.08-2.64); age 1.04 (1.02-1.06).
Conclusions: A low ABI had specificity of 99.7%; however, because of its low sensitivity (64%), we should consider CAD risk factors associated with a low ABI in order to use it as a first-line screening test.
Case Report(s)
-
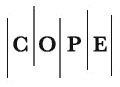
Behcet’s disease is a rare immune mediated systemic vasculitis which besides it’s more frequent involvement of eyes and skin, sometimes present with aortic pseudo aneurysm and more rarely cardiac inflammatory masses.A 51-year-old patient with Behçet’s Disease presented with two symptomatic aortic pseudoaneurysms concomitant with a right atrial mass. Computed tomography (CT) revealed one supra-celiac and another infrarenal aortic pseudoaneurysms. Echocardiography showed a large mobile mass in the right atrium. Both pseudoaneurysms were successfully excluded simultaneously via endovascular approach with Zenith stent-grafts, and the atrial mass was surgically removed 10 days later. Post-implant CT showed successful exclusion of both pseudo-aneurysms, patency of all relevant arteries, and patient is now asymptomatic and has returned to normal lifestyle. Multiple pseudoaneurysms concomitant with a right atrial mass can be an initial manifestation of Behçet’s disease. Endovascular repair can be a good treatment option for the pseudoaneurysms.
-
Pseudoaneurysms of the ascending aorta, which are rare and life-threatening complications in cardiovascular surgeries, can be caused by the Bentall procedure. We describe a 44-year-old woman, who had a medical history of acute aortic dissection (Type A) and the Bentall procedure and was admitted because of exertional dyspnea, edema of the lower extremities, ascites, and holosystolic murmur in the left lower sternal border. Preoperative echocardiography revealed a pseudoaneurysm of the ascending aorta and fistulization of the pseudoaneurysm to the right atrium. Multi-slice computed tomographic scan also showed a large pseudoaneurysm of the ascending aorta around the tube graft. The patient underwent surgery, during which the pseudoaneurysm was resected, the ostium of the right coronary artery was reimplanted, and the orifice of the right atrial fistula was sutured. Intraoperative transesophageal echocardiography revealed the perfect result of the surgery. The patient was discharged uneventfully.
-
Central venous catheter (CVC) insertion is a practical way to assess patients hemodynamic specially in cardiovascular surgery but this relatively simple junior level procedure is not risk free and its common reported complications include; pneumothorax, hydrothorax, hemothorax, local hematoma, cardiac tamponade, vascular injury, thrombosis, embolism, and catheter disruption. Here in this article we are going to present 6 patients with very unusual presentation of CVC complication which was neurological deficit presented by agitation , unconsciousness, disorientation to time and place and hemiparesis. All patients undergone neurologic consult and brain computed tomography. Final diagnosis was brain ischemic damage and finally we kept them on conservative management; fortunately we did not have any permanent damage.
-
Carney Syndrome (CS) is an autosomal dominant multiple neoplasia syndrome that includes cardiac, endocrine, cutaneous, and neural tumors. Cardiac myxomas can be seen in the course of CS. A 46-year-old female patient was admitted to our clinic with palpitation, cough, and exertional dyspnea. Physical examination revealed pigmented lesions, especially scattered in the neck, chest, and extremities. Echocardiography revealed a left atrial mass, 6 × 4 cm in size, originating from the interatrial septum that was protruding into the left ventricle through the mitral valve during diastole. The tumor was excised from the interatrial septum with its pedicle. The patient was discharged at the fifth postoperative day without any complication. Cardiac myxomas are a cornerstone of this disease since cardiac manifestations and related complications account for the majority of mortality seen in the course of CS.
Photo Clinic
-
A 51-year-old man was admitted to the emergency department with palpitation and atypical chest pain. He had a history of percutaneous mitral valve commissurotomy 20 years previously. He did not use any drugs. Physical examination was unremarkable except for a loud S1 on auscultation. The surface electrocardiogram (ECG) showed atrial fibrillation rhythmwith rapid ventricular response and right bundle branch block. Transthoracic and transesophageal echocardiographic examinations revealed normal left ventricular size with mild systolic dysfunction, ejection fraction of 45%, and moderate rheumatic mitral stenosis with mild to moderate mitral regurgitation. Also, there was a highly mobile multilobulated mass attached to the anterior wall of the left atrial appendage with a long stalk, simulating myxoma. The patient was referred for emergent surgery, during which the mass was removed. Pathological examination demonstrated organized thrombosis. Recently, Peters and et al.1 described a woman with significant mitral stenosis and a mass in the left atrium attached to the interatrial septum through a stalk; pathological examination showed thrombosis. In another report, a man with moderate mitral stenosis and a left atrial mass attached via a narrow stalk to the interatrial septum was described.2 In cardiac magnetic resonance imaging, thrombus often appears as a hypointense structure after the administration of intravenous gadolinium, whereas atrial myxomas show contrast enhancement. This imaging modality, however, is far from perfect.3