Vol 6 No 1 (2011)
Articles
-
The management of carotid artery stenosis reduces the risk of stroke and its related deaths. Management options include risk factor modification and medical therapy, carotid endarterectomy (CEA), and carotid artery stenting (CAS). Although several randomized controlled trials (RCTs), mostly conducted in late-1980s and mid-1990s, have proved CEA to be effective in the prevention of ipsilateral ischemic events in selected patients with carotid artery stenosis, aggressive risk factor modification and medical therapy with recently introduced antiplatelet agents, statins, and more effective antihypertensive medications may have reduced compelling indications for immediate surgery in asymptomatic populations. Also recently, due to improvements in percutaneous techniques and carotid stents, CAS has received wide attention as a potential alternative to CEA. Herein, we review the recent data on the management options of carotid artery stenosis and seek to identify the most appropriate treatment strategy in selected patients with carotid artery stenosis.
-
Background: Nowadays, developed junctional rhythm (JR) that occurs during slow-pathway radiofrequency (RF) catheter ablation of atrioventricular nodal reentrant tachycardia (AVNRT) has been focused upon as a highly sensitive surrogate end point for successful radiofrequency ablation. This study was conducted to assess the relationship between the presence and pattern of developed JR during the RF ablation of AVNRT and a successful outcome.
Methods: Seventy-five patients aged between 14 and 88 who underwent slow-pathway RF ablation due to symptomatic AVNRT were enrolled into the study and received a total of 162 RF energy applications. Combined anatomic and electrogram mapping approach was used for slow-pathway RF ablation. The ablation procedure consisted of 60-second, 60 °C temperature-controlled energy delivery. After each ablation pulse, successful ablation was assessed according to the loss of AVNRT inducibility via isoproterenol infusion. Four different patterns were considered for the developed JR, namely sparse, intermittent, continuous, and transient block. Success ablation rate was assessed with respect to the position, pattern, and number of junctional beats.
Results: Successful RF ablation with a loss of AVNRT inducibility was achieved in 43 (57.3%) patients using 119 RF energy applications (73.5%). JR developed in 133 of the 162 (82.1%) applications with a given sensitivity of 90.8% and low specificity of 41.9% as an end point of successful RF ablation, with a negative predictive value of 62.1%. The mean number of the developed junctional beats was significantly higher in the successful ablations (p value < 0.001), and the ROC analysis revealed that the best cut-off point of the cumulative junctional beats for identifying accurate AVNRT ablation therapy is 14 beats with 90.76 % sensitivity and 90.70% specificity. There were no significant differences in terms of successful ablation rates according to the four different patterns of JR and its positions (p value=0.338, p value=0.105, respectively) in the univariate analyses.
Conclusion: JR is a sensitive but non-specific predictor of the successful RF ablation of AVNRT. Nevertheless, according to the results, its specificity could increase with the presence of more than 14 cumulative junctional beats. Although the development of JR during slow-pathway RF ablation seems not to be reliable as a success end point, its absences could be a marker of requiring more energy application to ablate the slow pathway. -
Background: Myocardial ischemia is one of several causes of prolonged QT dispersion. The aim of this study was to evaluate the effect that percutaneous coronary intervention has on the depolarization and repolarization parameters of surface electrocardiography in patients with chronic stable angina.
Methods: We assessed the effects of full revascularization in patients with chronic stable angina and single-vessel disease who underwent percutaneous coronary intervention. Twelve-lead electrocardiograms were recorded before intervention and 24 hours subsequently. We measured parameters including QRS duration, QT and corrected QT durations, and JT and corrected JT duration in both electrocardiograms and compared the values.
Results: There were significant differences between the mean QRS interval (0.086 ± 0.01sec vs. 0.082 ± 0.01 second; p value = 0.01), mean corrected QT dispersion (0.080 ± 0.04 sec vs. 0.068 ± 0.04 sec; p value = 0.001), and mean corrected JT dispersion (0.074 ± 0.04 sec vs. 0.063 ± 0.04 sec; p value = 0.001) before and after percutaneous coronary intervention. No significant differences were found between the other ECG parameters.
Conclusion: Our data indicate that the shortening of corrected QT dispersion and corrected JT dispersion in patients undergoing percutaneous coronary intervention is prominent. -
Background: The right ventricular (RV) dyssynchrony has not been studied extensively and the existing literature has established the effect of cardiac resynchronization therapy (CRT) on the left ventricular (LV) dyssynchrony, but there is a dearth of data on the effect of CRT on the forgotten ventricle. We sought to evaluate the presence of mechanical right ventricular dyssynchrony in patients with systolic heart failure, selected for CRT, and track the changes early afterward utilizing the longitudinal strain analysis.
Methods: Thirty-six patients with severe left ventricular systolic dysfunction, candidated for CRT, were enrolled in this study. Mechanical dyssynchrony was assessed using tissue Doppler echocardiography. The time interval between the onset of the QRS to the peak systolic longitudinal strain at the RV free wall and the septum was obtained. The RV mechanical delay was calculated as the absolute value of the difference in the time-to-peak measurements between the RV and septum. The RV dyssynchrony was defined as the calculated delay in strain imaging, which was ± 2 SD above the mean value for the control subjects (20 cases). The RV function was evaluated using the RV fractional area change (RVFAC), tricuspid annulus plane systolic excursion (TAPSE), and peak systolic strain values of the RV free wall. Four to 7 days after CRT implantation, echocardiographic reevaluations were done.
Results: The calculated cut-off value for the RV dyssynchrony was 41.5 msec, according to which the pre-CRT analysis specified two patient groups: Group 1 (16 cases) with RV dyssynchrony and Group 2 (20 patients) without RV dyssynchrony. Significant improvement in the RV dyssynchrony was noted in Group 1 after CRT (30 ± 28.9 msec vs. 68.8 ± 21 msec; p value < 0.01 vs. 14 ± 10 msec vs. 19 ± 16.5 msec; p value = 0.18 respectively). A significant correlation was found between the severity of the RV dyssynchrony and peak systolic strain in the RV free wall (r = -0.5; p value < 0.05). No significant relation was found between the RV dyssynchrony and right ventricle fractional area change (RVFAC), LV mechanical dyssynchrony, time-to-peak systolic strain in the RV free wall, QRS width, or morphology. In Group 1, the peak systolic strain increased insignificantly (p value = 0.15 for the basal segment; p value = 0.20 for the mid segment). A moderately significant correlation was found between the RV mechanical delay before CRT vs. the post-CRT values (r = 0.4; p value = 0.01).
Conclusion: Early after CRT, the RV mechanical delay can improve and the significant improvement is seen in patients with baseline RV mechanical dyssynchrony. -
Background: Redo coronary artery bypass grafting surgery (CABG) is associated with a higher risk of mortality than the first operation. However, the impact of percutaneous coronary intervention (PCI) on the outcome in such patients is currently unclear. We evaluated the in-hospital and six-month clinical outcomes of post-CABG patients who underwent PCI in our center.
Methods: Between April 2008 and July 2009, 71 post-CABG patients (16 women and 55 men) underwent 110 stent implantations (74% drug-eluting stents) for 89 lesions. Sixty percent of the PCI procedures were performed on the native coronary arteries, 32% on graft arteries, and 8% on both types of vessels. Major adverse cardiac events (MACE) were recorded in hospital and at six months’ follow-up.
Results: The procedural success rate was 93%, and the in-hospital MACE rate was 5.6 % (1 death, 3 myocardial infarctions). At 6 months, the incidence of MACE was 5.6% (no death or myocardial infarction, but 4 target lesion revascularizations) and 4 (5.6 %) in-stent restenoses. There was no statistically significant difference in the comparison of MACE between the patients treated in either native arteries or in the grafts (15% vs.12%, p value = 0.8). According to the univariate analysis, hypertension and the use of the bare metal stent vs. the drug-eluting stent were the significant predictors of MACE, whereas the multivariate analysis showed that only hypertension (OR = 3.7, 95% CI 3.4-4, p value < 0.048) was the independent predictor of MACE. The mean of the left ventricular ejection fraction had no effect on the incidence of MACE (p value = 0.9). The multivariate analysis showed hypertension (p value < 0.048) and the use of the bare metal stent (p value < 0.018) were the independent predictors of MACE. The chronic total occlusion (CTO) (p value < 0.01) was the independent predictor of the success rate. The prevalence of diabetes had no impact on the incidence of MACE according to the univariate analysis (p value = 0.9). Our multivariate analysis showed that hypertension and the use of the bare metal stent were the independent predictors of MACE and that chronic total occlusion was the independent predictor of the procedural failure rate.
Conclusion: PCI is preferable to redo CABG for post-CABG patients. The independent predictors of MACE were hypertension and bare metal stents. -
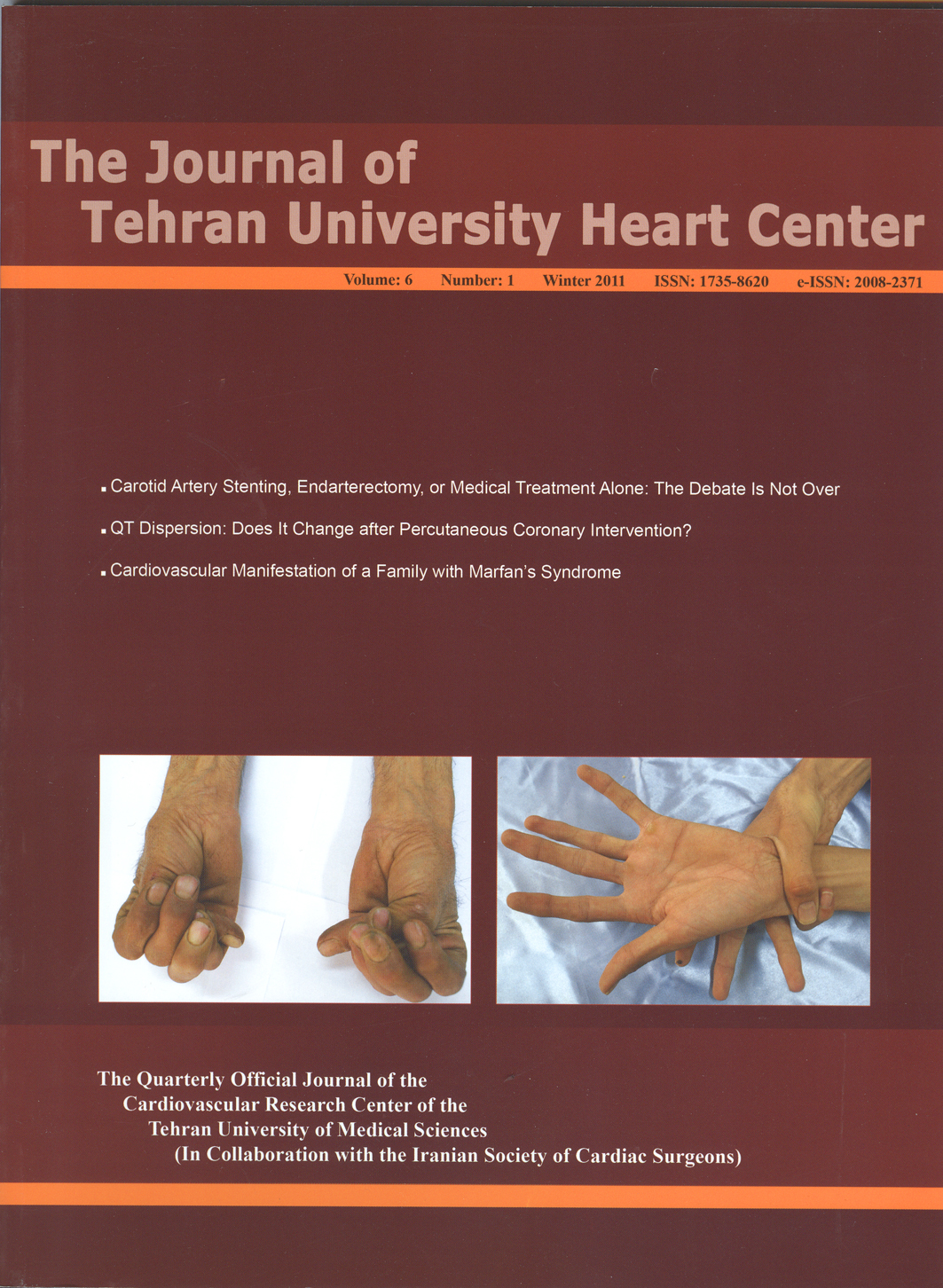
Marfan’s syndrome (MFS) is a genetic disorder associated with autosomal dominant inheritance. In MFS, the most prevalent cause of death is cardiovascular involvement. Here we introduce a family with a severe penetration of MFS. Eleven members of this family have MFS (father, two daughters, three sons, and five grandchildren). The most common cardiac involvement in our patients was mitral valve prolapse as manifested by mitral regurgitation. At ten years’ follow-up, two patients had aortic root dilatation running the risk of aortic dissection; they were, therefore, scheduled for cardiac surgery, during which the Bental procedure was successfully performed. Fortunately, all of the members of this family are currently alive.
-
A pulmonary embolus clogs the artery that provides blood supply to a part of the lung. The embolus not only prevents the exchange of oxygen and carbon dioxide but also decreases blood supply to the lung tissue itself, potentially causing the tissue to die (infarct). A 52-year-old man presented with syncope and anxiety. He had sinus tachycardia and dilated right ventricle with trabeculations. A differential diagnosis of arrhythmogenic right ventricular dysplasia and pulmonary embolism prompted CT angiography, which revealed a bilateral massive pulmonary embolism. The patient was treated successfully with thrombolytic drugs.
-
Primary cardiac tumors are quite rare, especially in the pediatric age group, and their atypical presentations often prevent a timely diagnosis. Most primary cardiac tumors in the pediatric age group are benign. Fibromas are generally reported as the second most common primary cardiac tumors in the pediatric age group. These neoplasms are often intramural and involve the left ventricular free wall or the interventricular septum. Although benign, fibromas may become life-threatening by causing arrhythmias or obstruction to the blood flow. A case of supravalvular intraluminal ascending aorta fibroma in a 23-month-old girl, presenting with syncope, is described here; the location is rare and the presentation atypical for this type of tumor. Transesophageal echocardiography helped us to evaluate the anatomic details of the tumor and plan surgery.