Vol 16 No 3 (2021)
Original Article(s)
-
Background: Angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs) are common hypertension medications. We aimed to investigate the association between treatment with ACEIs/ARBs and disease severity and mortality in patients with hypertension hospitalized for coronavirus disease 2019 (COVID-19).
Methods: Information from the medical records of 180 hospitalized patients diagnosed with COVID-19 infection admitted in 2020 to Loghman Hakim Hospital, Tehran, Iran, was collected. Clinical histories, drug therapies, radiological findings, hospital courses, and outcomes were analyzed in all the patients. The demographic and clinical characteristics of the patients were also analyzed, and the percentage of patients with hypertension taking ACEIs/ARBs was compared between survivors and nonsurvivors.
Results: The study population consisted of 180 patients at mean±SD age of 67.76±18.72 years. Hypertension was reported in 72 patients (40.0%). Patients with hypertension were older than those without it (mean±SD age =72.35±12.09 y). Among those with hypertension, death occurred in 33 patients (45.8%), of whom 60.6% were men. Fifty-three patients (73.6%) with hypertension were on ACEIs/ARBs. The ACEIs/ARBs group had a significantly lower mortality rate than the non-ACEIs/ARBs group (37.7% vs 68.4%; OR: 0.192; 95% CI: 0.05–0.68; P=0.011).
Conclusion: This single-center study found no harmful effects associated with ACEIs/ARBs treatment. Patients on ACEIs/ARBs had a lower rate of mortality and disease severity than the non-ACEIs/ARBs group. Our study supports the current guideline to continue ACEIs/ARBs in patients with hypertension.
-
Background: Pain management after sheath removal is one of the most significant points in patient care. The use of a simple, practical, and combined method in this field is essential. The purpose of this study was to evaluate the efficacy of an intervention program for pain intensity reduction in patients undergoing arterial sheath removal after coronary artery angioplasty.
Methods: This semi-experimental study was conducted in 2020 on 90 eligible patients selected via the purpose-based method and randomly assigned to experimental and control groups. The intervention program for the experimental group included training to relax the abdominal muscles, deep and slow breathing, and precise pressure on the femoral pulse. Pain intensity was measured before, during, and several times after arterial sheath removal. The independent t, Fisher exact, and χ2 tests were used to analyze the data.
Results: Women comprised 66.6% of the study participants, who had a mean age of 58.20±8.70 years. No significant differences were observed concerning pain intensity, bleeding, pseudoaneurysm formation, and hematoma between the 2 groups before the intervention (P=0.531). However, during the intervention and in the fifth and tenth minutes after the intervention, pain intensity was lower in the experimental group (P<0.050), whereas no such differences were observed regarding bleeding, pseudoaneurysm formation, and hematoma.
Conclusions: Given the effectiveness of our intervention program in ameliorating pain intensity and vasovagal response after arterial sheath removal, we suggest that this program, along with prescription drugs, be used for the management of patients’ pain.
-
Background: Behcet’s disease (BD) is a vasculitis with multisystem and multiorgan involvement. Cardiac involvement in BD is a rare complication with a poor outcome that manifests itself in different forms. In this study, we aimed to investigate cardiac involvement in BD.
Methods: This is a retrospective study based on cardiac manifestations in BD according to the data of the Behçet’s Disease Unit, the Rheumatology Research Center, Tehran University of Medical Sciences, from registered patients from 1975 until June 2017. Cardiac manifestations consisted of pericarditis, myocardiopathy, myocardial infarction, stable ischemic heart disease, endomyocardial fibrosis, thrombosis, and valvular and coronary involvement. All the patients’ baseline and demographic data were recorded in a designed questionnaire. The laboratory workups, imaging, and pathological tests were also performed.
Results: We studied 7650 patients with BD, of whom 51% were male. In the entire study population, 47 patients manifested cardiac involvement: valvular involvement in 6.1%, myocardial infarction in 23.4%, stable ischemic heart disease in 20%, pericarditis in 21.3%, intracardiac thrombosis in 2.1%, coronary aneurysm in 2.1%, heart failure in 12.8%, and dilated cardiomyopathy in 4.3%.
Conclusion: The prevalence of cardiac involvement in our patients with BD was 0.6%. A multidisciplinary approach can reduce mortality and morbidity rates. Consequently, we suggest that echocardiography and other cardiac diagnostic tests be routinely considered for early diagnosis and subsequent treatment.
-
Background: The discharge of uncomplicated patients with ST-segment-elevation myocardial infarction (STEMI) within 48 to 72 hours has been proven safe and feasible. The safety and feasibility of the very early discharge (≤48 h) of such patients, especially during the COVID-19 pandemic with limited bed availability and infection risk, have yet to be evaluated.
Methods: In this cohort study on 108 patients with STEMI who presented to Farshchian Heart Center between February and May 2020, 30 patients received fibrinolysis and 78 were scheduled for emergent coronary angiography. One patient had no coronary obstruction, 3 underwent emergent surgery, and 3 had high-risk features mandating a prolonged stay. The remaining patients were assigned to either Group A (≤48 h) or Group B (>48 h) regarding hospital discharge. Demographic, angiographic, procedural, and outcome data were compared between the 2 groups.
Results: Group A consisted of 51 patients, including 7 women (13.7%), at a mean age of 62.74±12.35 years, and Group B comprised 20 patients, including 4 women (20.0%), at a mean age of 65.20±12.82 years. The mean hospital length of stay was 38.02±9.15 hours in Group A and 88.20±23.31 hours in Group B (P<0.001). The mean stent diameter was smaller in Group B (3.19±0.34 mm vs 2.96±0.29 mm; P=0.008). Demographic, angiographic, procedural, and outcome data, including the rates of in-hospital, 1-week, and 1-month mortality, were similar between the 2 groups.
Conclusion: This study shows that a hospital discharge in less than 48 hours in low-risk patients with STEMI is safe and feasible. The potential advantages of this approach in the COVID-19 pandemic should be balanced against its risks.
Case Report(s)
-
The basic components of energy drinks include caffeine, guarana, taurine, ginseng, and sugar. The excessive consumption of energy drinks has been associated with cardiovascular events such as tachycardia and myocardial infarction in the literature. We herein describe a 24-year-old man admitted to the emergency department. The patient’s medical history and family history were unremarkable. It was, however, learned that he had consumed 8 to 10 cans of energy drinks per day (3.5–4 Lit/d) in the 2-week period leading to the hospital admission. Physical examination revealed bilateral diffuse rales and 2+ pretibial edema. Echocardiography showed a left ventricular ejection fraction of 25% with global left ventricular hypokinesia and dilated left ventricular dimensions. Coronary angiography demonstrated normal coronary arteries. On cardiac magnetic resonance imaging, the left ventricle was dilated, and the systolic function was reduced. No pathological enhancement was observed. This case report and many previous studies support a possible link between caffeinated energy drinks and cardiovascular events.
-
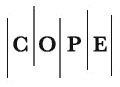
Longitudinal stent deformation (LSD) is a recently reported problem with newer generation stents. The modification of stent materials and designs to make them more deliverable and conformable, as well as a focused approach in retaining their radial strength, has compromised longitudinal strength in currently available stents. Additionally, enhanced stent radiopacity, improved fluoroscopy, and heightened awareness have led to an increased incidence rate of the potentially under-recognized problem of LSD. Although originally described in deployed stents, LSD is being recognized in undeployed stents too. With available data to suggest an increased rate of adverse cardiac events like stent thrombosis and in-stent restenosis with LSD in deployed stents, an attempt to retrieve an undeployed deformed stent appears justified. We report 3 cases of LSD in undeployed stents and discuss its recognition. We also discuss the retrieval and visual inspection of retrieved stents and the simultaneous completion of coronary interventions via a double guide technique.
-
Temporary pacemaker wires are commonly used for the diagnosis and treatment of arrhythmias in the acute postoperative period. We herein describe a 65-year-old woman with a history of coronary artery bypass graft surgery who was referred to the hospital with a purulent discharge in the lower third of the sternal region while on antibiotics. Two years later, following treatment failure, 2 sternal wires were removed. Several years after the surgery, the patient developed a purulent discharge. On suspicion of rib osteomyelitis, the last left cartilage attached to the sternum was excised and removed together with an infectious tract.
During the operation, the right ventricle was torn, and tampons were used to control bleeding. The patient was placed under cardiopulmonary bypass via the cannulation of the left femoral artery and the right femoral vein. The sternum was opened, and the rupture site was repaired. A temporary epicardial pacing wire was found at the site of the right ventricular rupture. Several days later, the patient was taken from the intensive care unit to the operating room due to a pulsatile hematoma in the left groin and a diagnosis of a pseudoaneurysm of the femoral artery. After a week, the purulent discharge at the lower sternum improved, and the patient was discharged. At 1 month’s post-discharge follow-up, the infection was eradicated.
Photo Clinic
-
-
Letter to the Editor
-
-